
The Barrett’s Oesophagus Registry and Biobank funded by The Oesophageal Cancer Fund’s fundraising efforts supports patients with Barrett’s Oesophagus by regularly monitoring their condition to prevent Oesophageal Cancer.
Prevention of Oesophageal Cancer is vital as well as Early detection of Oesophageal Cancer.

The symptoms of Barrett’s Oesophagus are persistent acid Indigestion or Heartburn or persistent reflux
There are nearly 9,000 people on the National Barrett’s Oesophagus Registry

The National Barrett’s Oesophagus Registry and Biobank provides important clinical and demographic information on Irish patients to allow for research into Barrett’s Oesophagus and Oesophageal Cancer
Barrett’s oesophagus occurs when persistent or long-term acid reflux damages the normal inner lining of the oesophagus. This process usually takes a long time to happen. Acid Reflux also called gastro-oesophageal reflux disease or GORD occurs when the stomach and small bowel acids and bile flow back up into the oesophagus.
Over time the lining of the oesophagus is damaged, the cells change and abnormal (or bad) cells can develop in the lining of the oesophagus (food pipe), it is not cancer, but a pre-cancerous condition known as Barrett’s Oesophagus. A small number of people (less than 1%) with Barrett’s Oesophagus go on to develop Oesophageal Cancer.
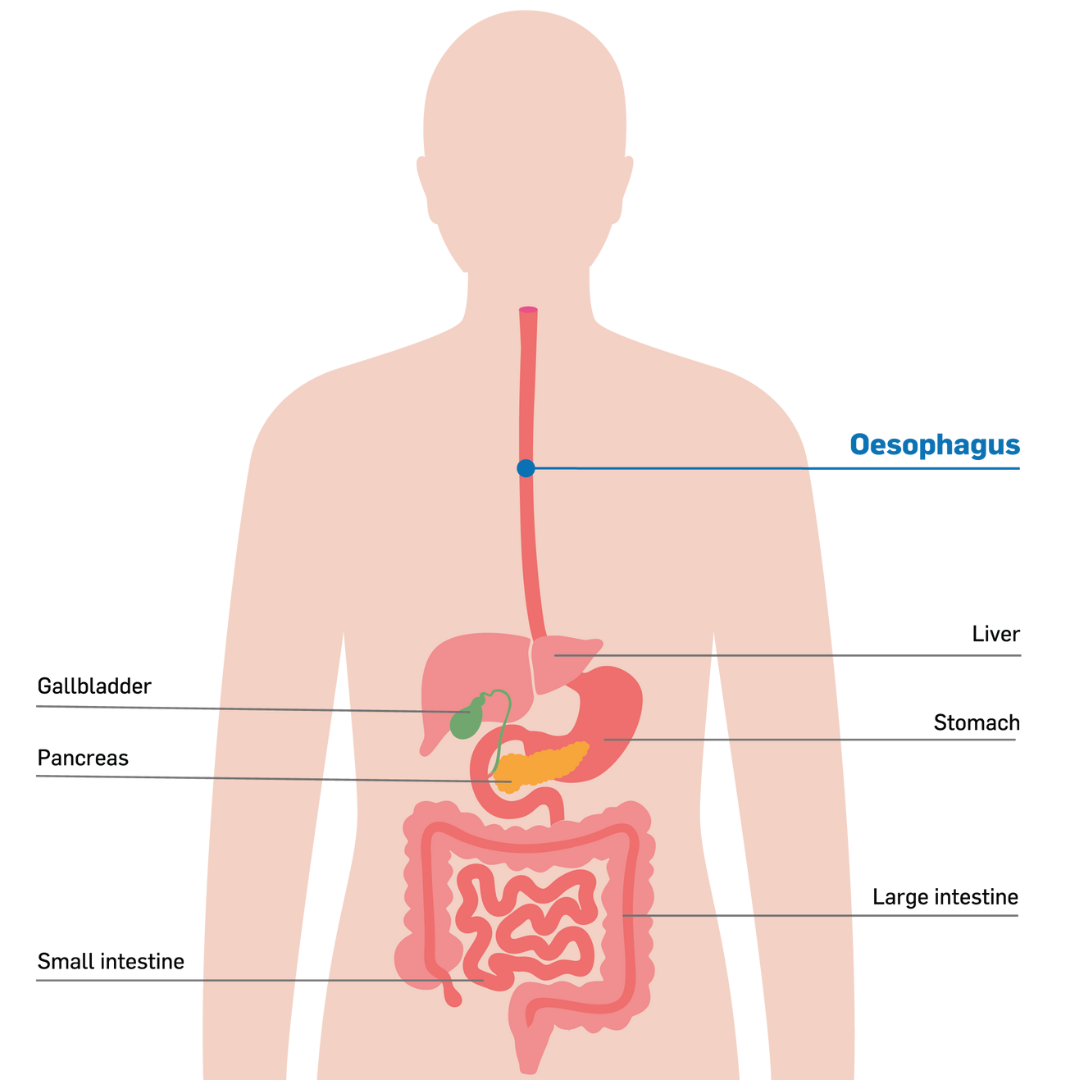
The Oesophagus is a part of the digestive system, a muscular tube that connects your mouth to your stomach and can sometimes be referred to as the gastro-intestinal tract or GI tract. The Oesophagus is usually between 25-30cm in length in adults. Food and liquid pass through the oesophagus. There is a muscle - the sphincter - at the top of the oesophagus that opens to allow food or liquid to pass to the stomach. This also functions to stop food or liquid from going down the windpipe.
The oesophagus joins the stomach at the lower part of the oesophagus at the gastro-oesophageal junction There are sphincter muscles close to the gastro-oesophageal junction to control food and liquids moving from the oesophagus to the stomach. This sphincter muscle then closes to stop the contents of the stomach and stomach acid moving backwards from the stomach into the oesophagus.
The oesophagus is made up of four layers:
The inner layer - the mucosa, is a moist layer that helps food to pass easily into the stomach.
The submucosa - a layer of the oesophagus with glands that produce mucus also keeping the oesophagus moist.
The muscular layer - the muscularis squeezes and pushes food down into the stomach.
The outer layer - the adventitia attaches the oesophagus to surrounding parts of the body.
The lining of the oesophagus is multi-layered and protects the oesophagus from injury caused by food, liquids, stomach acid and bile. When long-term persistent acid reflux or GORD damages the inner lining of the oesophagus. The cells lining the Oesophagus - the squamous cells - that are normally flat change in shape, a process called metaplasia.
This exposure to acid and bile can also injure the lining of the oesophagus and may cause inflammation of the oesophagus called oesophagitis. In some cases, as healing occurs, the normal lining of the oesophagus is replaced by changed cells that resemble those in the stomach or intestine. It is this abnormal lining that is called Barrett’s oesophagus.
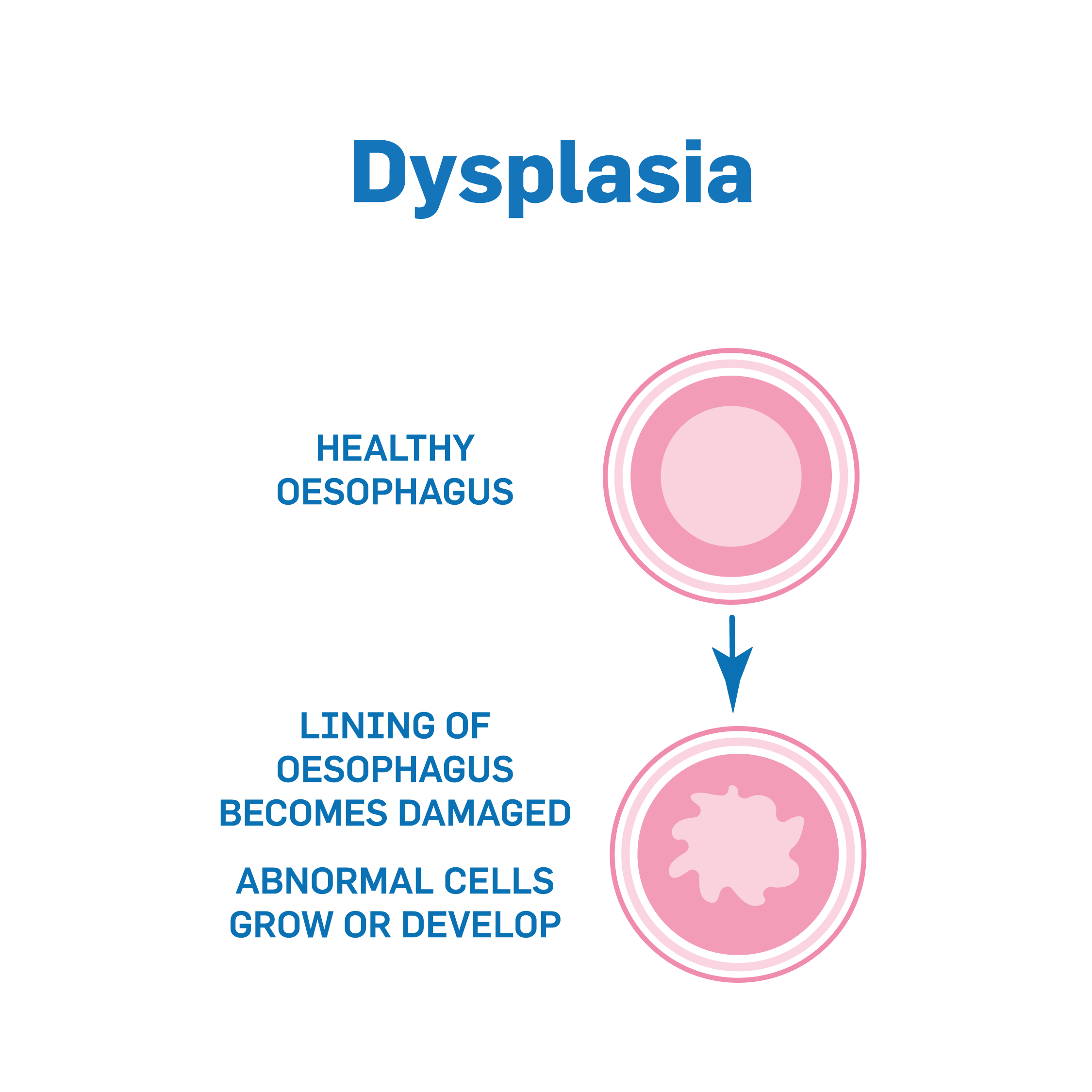
Dysplasia
Sometimes the cells of Barrett’s Oesophagus can become more abnormal. Cells that begin to show abnormal changes may gradually be developing a condition called dysplasia. This is why many people with Barrett’s oesophagus have regular monitoring. Dysplasia is often divided into 2 grades based on how abnormal the cells appear under the microscope: low-grade and high-grade. Your doctors will carry out tests to determine the grade of the dysplasia.
low grade dysplasia – this means the cells are slightly abnormal
high grade dysplasia – this means the cells are more abnormal.
People who have Barrett’s Oesophagus with dysplasia have a small increase in their risk of Oesophageal cancer, but most do not go on to get Oesophageal Cancer.
In some cases the dysplasia can develop further a small number of people (less than 1%) with Barrett’s Oesophagus go on to develop Oesophageal Cancer.
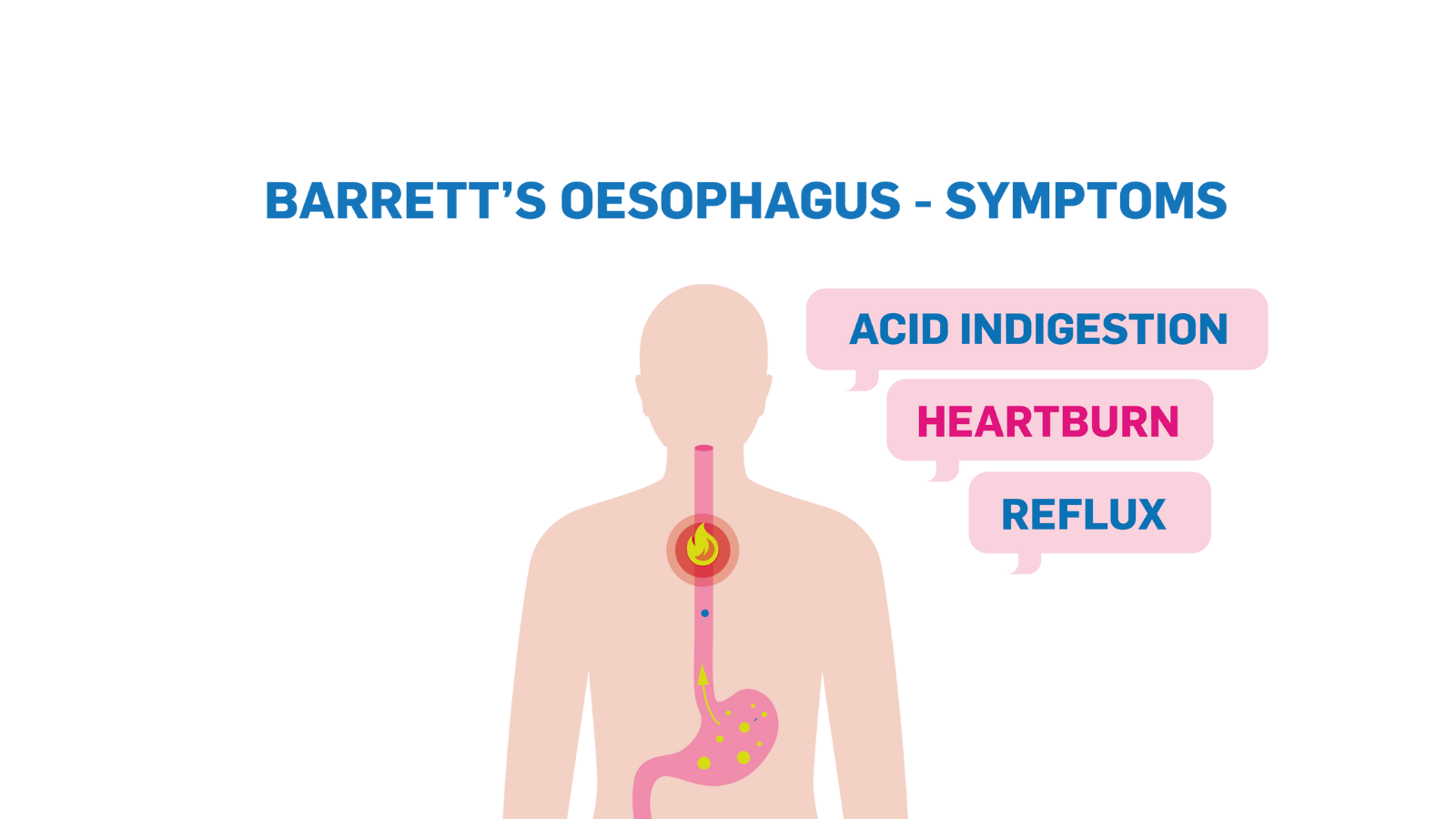
The main symptoms of Barrett’s Oesophagus are persistent acid reflux or gastro-oesophageal reflux disease (GORD). People with persistent acid reflux or GORD often experience heartburn and indigestion. Acid Reflux is very common, and many people have symptoms at some point in their lives. However, persistent acid reflux and heartburn or indigestion over a long period of time can damage the oesophagus and cause Barrett’s Oesophagus.
Acid reflux occurs when stomach acid constantly flows back up into the oesophagus. As a long-term, persistent condition, the acid can irritate the oesophagus, causing pain, heartburn and indigestion. In some people, the valve that joins the oesophagus to the stomach is weak. This means stomach acid moves up more easily into the oesophagus. Approximately 1 in 10 people (10%) undergoing an endoscopy for acid reflux have Barrett’s Oesophagus.
If you’re experiencing the symptoms of Barrett’s Oesophagus persistent acid reflux over a long time, indigestion and heartburn, or notice yourself constantly reaching for heartburn medication, then you should consult your GP.
Having one or more risk factors can increase your risk of developing acid reflux. Not everyone with acid reflux develops Barrett's oesophagus. it is more likely to develop for people who have had severe acid reflux for many years. Other risk factors associated with Barrett’s Oesophagus include;
Being Overweight
Being overweight can significantly increase your risk because other factors like long-term reflux, heartburn and/or indigestion are more common in people who are overweight.
Eating spicy, fatty acidic foods
Eating spicy, acidic or fatty foods regularly can produce more acid in the stomach and increase the risk of acid reflux. Persistent acid reflux can affect the lining of the oesophagus over time and lead to Barrett’s Oesophagus. Smoking and alcohol
Smoking increases the risk of both Barrett’s Oesophagus and Oesophageal Cancer the longer a person smokes for and the more they smoke. All types of smoking are very harmful.
Your risk of Barrett’s Oesophagus increases if you drink more than 14 units of alcohol a week.Drinking a lot of alcohol over a long period of time also increases your risk of developing Oesophageal Cancer.
Age
Typically people over the age of 50 are at a higher risk of developing Barrett’s Oesophagus. However, increasingly Barrett’s Oesophagus can occur for people in younger age brackets. It is important that anyone experiencing the symptoms of Barrett’s Oesophagus seeks advice from their GP.
Gender
More men than women are affected by Barrett’s Oesophagus. Although women are also at risk of developing this condition.. Hiatus hernia
A hiatus hernia is when part of the stomach moves up through the diaphragm, into the chest space. The diaphragm is the muscle that divides the abdomen or stomach area from the chest. It also helps to keep acid in the stomach.
One of the main symptoms you may experience from a hiatus hernia is acid reflux. Acid reflux causes pain and discomfort during and after eating certain foods. Persistent acid reflux can damage the oesophagus over time and lead to Barrett’s Oesophagus.
Barrett’s Oesophagus is diagnosed by examining the oesophagus using an endoscopy. A sample of cells (biopsy) may be taken, and your GP may suggest regular endoscopies to detect any changes to cells in the oesophagus. If pre-cancerous changes (dysplasia) develop, then treatment to remove or destroy the pre-cancerous cells may be advised.
It’s worth noting that Barrett’s Oesophagus is generally managed without surgery, with treatment focused on reducing reflux, controlling symptoms and most especially, preventing Oesophageal Cancer. Lifestyle changes, coupled with certain medications, can help reduce stomach acid.
Biopsy
A biopsy involves the removal of a small amount of tissue from an area where there are suspected abnormalities. The tissue sample is then sent to the laboratory for analysis.
A biopsy may be carried out during an endoscopy. An endoscopy is a test using a long flexible tube with a camera that examines the lining of your oesophagus for anything that looks abnormal in the area. Sedation is used during endoscopies where you will be given medication to become more relaxed or sleepy.
Endoscopy
Endoscopies can also be used to take biopsies of any tissues in the oesophagus. These tissues are then tested to identify any abnormalities.
Following your endoscopy your doctor will speak to you about how the test went and the next steps. You should check how long they expect the results to take and who you should contact for the results. This may be the hospital or your GP.
The National Barrett’s Oesophagus Registry and Biobank was set up to monitor and survey patients presenting with Barrett’s Oesophagus. Apart from the goal of increasing the early diagnosis of Oesophageal Cancer, this National Barrett’s Oesophagus Registry helps improve services and information for patients.
In accordance with international guidelines, it also allows Consultants to see if changes in the management of patients should be altered.
Through this OCF-funded programme, collaborations have been formed with leading international groups in Barrett’s Oesophagus and Oesophageal Cancer.
The National Barrett’s Oesophagus Registry is an essential database that was established in 2009 to meet The Oesophageal Cancer Fund’s aim of combating Oesophageal Cancer through early detection. To date, over €1.5 million in funding has gone towards keeping the National Barrett’s Registry alive, employing Registry personnel and linking six national hospitals: St. James’s, St. Vincent’s, Beaumont, Mater Misericordiae, Dublin, Mercy Hospital, Cork and University Hospital Galway.
Since 2009 there have been nearly 9,000 patients recorded on the Barrett’s Registry. Though not cancerous, Barrett’s Oesophagus is a condition that is frequently a precursor to full-scale Oesophageal Cancer. The Registry helps the medical professionals identify at-risk patients earlier and track their progress using endoscopies and bioscopies. Cellular changes such as dysplasia and or cancer can be diagnosed much earlier, meaning Oesophageal Cancer can be addressed in its early and most treatable phase. The data manager records and monitors a range of follow-up data for all Registry patients across all six hospital sites. Barrett’s patients who show progression in their disease are offered Radio Frequency Ablation (RFA) therapy, a highly effective Halo procedure that eradicates diseased tissue and allows healthy new tissue to regenerate. The Barrett’s Oesophagus Registry is now part of the UK Radio Frequency Ablation Registry that covers 26 hospitals of which St. James’s Hospital Dublin is the third largest contributing centre.
OCF donations also finance a National Barrett’s Bio Bank that operates in tandem with the National Barrett’s Registry. Tissue and blood samples from consenting Barrett’s patients are collected, stored and used for vital patient-focused research that is helping medical professionals to better understand what factors drive progression to Oesophageal Cancer. Many scientific studies which have utilised this national biobank have been submitted for publication.
Thanks to the fundraising efforts of The Oesophageal Cancer Funds amazing donors and supporters, scientists and clinicians can now draw upon this invaluable collection of tissue and blood samples, to carry out life saving research into Oesophageal Cancer and Barrett’s Oesophagus.
Carmel recognised that something was not right with her husband Gerry when, during her pregnancy, she found that he was using more antacids than she was for his ongoing heartburn, which had become persistent.
Gerry was diagnosed with Barrett’s Oesophagus after a GP referral for an endoscopy and was added to the National Barrett’s Registry, where his condition was monitored regularly. Unfortunately, Gerry did go on to develop Oesophageal Cancer but thanks to regular monitoring and screening, Gerry’s cancer was identified early and he is now cancer free.
